AbstractThe technique of stem cells or hepatocytes transplantation has recently improved in order to bridge the time before whole-organ liver transplantation. In the present study, unfractionated bone marrow stem cells (BMSCs) were harvested from the tibial and femoral marrow compartments of male mice, which were cultured in Dulbecco's modified Eagle's medium (DMEM) with and without hepatocyte growth factor (HGF), and then transplanted into Schistosoma mansoni-infected female mice on their 8th week post-infection. Mice were sacrificed monthly until the third month of bone marrow transplantation, serum was collected, and albumin concentration, ALT, AST, and alkaline phosphatase (ALP) activities were assayed. On the other hand, immunohistopathological and immunohistochemical changes of granuloma size and number, collagen content, and cells expressing OV-6 were detected for identification of liver fibrosis. BMSCs were shown to differentiate into hepatocyte-like cells. Serum ALT, AST, and ALP were markedly reduced in the group of mice treated with BMSCs than in the untreated control group. Also, granuloma showed a marked decrease in size and number as compared to the BMSCs untreated group. Collagen content showed marked decrease after the third month of treatment with BMSCs. On the other hand, the expression of OV-6 increased detecting the presence of newly formed hepatocytes after BMSCs treatment. BMSCs with or without HGF infusion significantly enhanced hepatic regeneration in S. mansoni-induced fibrotic liver model and have pathologic and immunohistopathologic therapeutic effects. Also, this new therapeutic trend could generate new hepatocytes to improve the overall liver functions.
INTRODUCTIONHepatic fibrosis occurs in the setting of chronic liver injury of different etiologies, including schistosomiasis. Schistosomiasis is an important cause of hepatic fibrosis. Chronic infection by Schistosoma mansoni is one of the experimental models of hepatic fibrosis used to elucidate the mechanism involved in the fibrogenic process [1]. Thus, it is of great interest to explore new therapeutic strategies to ameliorate the damages caused by fibrogenesis in chronic liver diseases [2]. Several studies reported that hepatic fibrosis is a reversible disease; therefore, an effective treatment would probably prevent or reverse the fibrotic process in the liver [3,4].
The key event in S. mansoni infection is the formation of granulomas around eggs trapped in the portal venules of the liver tissue [5], and the eggs release a variety of substances, leading to antigen-specific humoral and cell-mediated immune responses [6] which is a complex pathophysiological cascade event which terminates in fibrosis and portal hypertension [7,8].
The granulomatous reaction results in a lesion 20 times larger than the egg itself. This reaction started with accumulation of T-cells which attract eosinophils and neutrophils around the living eggs to destroy the egg shell. Consequently, following initiation of the inflammation, macrophages secrete proinflammatory molecules such as IL-1, IL-6, and TNF-α [9]. Also, collagen is a group of naturally occurring proteins, and it is the main protein of connective tissues making about 25-35% of the whole body protein content [10]. Excessive production of collagen has been documented in proliferative disorders such as liver cirrhosis. In other clinical situations such as tissue repair and wound healing, the overproduction and deposition of collagen are required to heal the damaged tissues. In order to understand the critical role of collagen in various pathophysiological conditions, it is necessary to determine its content in liver tissues [11].
Stem cells were reported to have a potential role to support tissue regeneration, requiring minimally invasive procedures with few complications. They have recently shown promise in cell therapy because they have the capacity for self-renewal, multilineage differentiation, and are applicable to human diseases [12]. Transplanted BMSCs were reported to give rise to hepatocytes and exert significant influence on hepatic architecture according to Abdel Aziz et al. [13]. Also, Pai et al. [14] stated that transplantation of BMSCs can restore liver mass and function, alleviate fibrosis, and correct inherited liver diseases. Therefore, it can significantly improve the liver functions (albumin, ALT, AST, and ALP) of patients with terminal liver diseases with good safety and effectiveness. So, regenerative medicine has emerged as an alternative therapy to improve the damaged liver [15,16,17].
MATERIALS AND METHODSExperimental animalsBALB/c mice were used for this experiment and bred at Theodor Bilharz Research Institute (TBRI), Egypt. Female mice were used as recipients while male mice were used as donors of BMSCs. All animal protocols were conducted in accordance with the valid international guidelines for animal experimentation and were approved by the TBRI's animal research committee.
Experimental designA total of 96 female BALB/c mice were divided into 4 main groups (24 mice/group). Group A contained normal uninfected negative control mice which had injected intravenously with saline; the animals of group B were infected subcutaneously with S. mansoni cercariae (obtained from infected Biomphalaria alexandrina snails which were bred and maintained at the SBSP/TBRI) and not subjected to bone marrow stem cells inoculation. The animals of groups C and D were infected with S. mansoni cercariae and subjected to treatment with BMSCs (1 million cells/mouse) alone and BMSCs in combination with HGF, respectively on the 8th week post-infection (PI). BMSCs derived from male BALB/c mice were infused by peripheral injection route.
Eight animals from each group were sacrificed after the first, second, and third month post-treatment (PT) and their livers were subsequently processed for histological and immunohistological examinations. The liver samples were fixed in 10% buffered formalin for histopathological study. Blood samples were taken individually for sera preparation, and kept at -20℃ until used for examinations.
Isolation, culture, purification, and inoculation of BMSCsSerum-free media were prepared using RPMI-1640, supplemented with L-glutamine, hepes buffer, sodium bicarbonate, and penicillin/streptomycin with pH 7.2-7.4. Then, complete media consisted of serum-free media supplemented with 20% fetal calf serum (FCS). BMSCs were harvested from the bone marrow of the femurs and tibiae of donor male mice according to the described method [18,19], with some modifications. Finally, the isolated cells were incubated for 48 hr at 37℃ under 5% CO2 for pre-stimulation of BMSCs. Cells viability was measured after 48 hr incubation and counted using a hemocytometer under graduated microsope. Then, a single intravenous inoculation of 1 million male unfractionated BMSCs was applied per mouse to the non-ablated female S. mansoni-infected mice of group C at week 8 PI. Also, another single inoculation with the same number of unfractionated BMSCs supplemented with HGF was injected intravenously into the non-ablated female S. mansoni-infected mice of group D at week 8 PI.
PCR detection of male derived BMSCsThe presence of donor-derived DNA in the liver tissue was analyzed after BMSCs transplantation in mice of all studied groups. The presence or absence of the sex determination region on the Y chromosome male (sry) gene in recipient female mice was assessed by PCR [18].
Hepatic histopathology and immunohistochemistry parametersLiver specimens were fixed in 10% formalin, processed to paraffin blocks, and sectioned at 4 µm thickness. Sections were stained with hematoxylin and eosin (H&E) to study the hepatic morphological changes and hepatic schistosomal fibrosis [19].
Liver sections were examined by a light microscope regarding the exerted hepatic schistosomal infection and portal fibrosis through the periods of the experiment [20]. This study focused on tracing the homing of the transplanted BMSCs and their differentiation into newly formed hepatocytes [19], applying immunohistochemistry techniques using monoclonal anti-mouse anti-OV-6 antibodies for detection of newly formed hepatocytes.
Measurement of granuloma diameterLiver tissue lesions from 5, 6 animals were measured for each group. Measurements were done only for granulomas containing a single egg in their center. The mean granuloma diameter (MGD) was obtained in microns by measuring 2 diameters of the lesion at right angles to each other with the help of an ocular micrometer. The count was done under a light microscope. The MGD of each liver granuloma was obtained in microns by dividing the sum of the measured vertical and transverse diameters of the lesions by 2. The mean diameter of all lesions measured was then calculated for each group [21]. According to the method [22], lesion counts from 50 to 100 were taken into considerations. Then, the percent suppression of MGD/treated group was calculated.
Measurement of granuloma numberGranuloma count was carried out at a low power magnification (×10) of serial tissue sections of more than 250 µm a part in all fields of liver sections. The mean number of granulomas was calculated for each mouse. The mean was calculated for each experimental group from the mean values of the individual mice. Granuloma structural configuration, including cellular components and associated histopathological changes was also studied [23].
Sirius red staining for collagenThe collagen content of the liver sections stained with Picrosirius red was evaluated quantitatively for the percentage areas of collagen using Computerized Cell Image Analysis. Collagen fibers within the squares of the ocular reticule were counted at ×200 magnification [24].
Detection of OV-6 in hepatic tissues using immunohistochemical techniqueThe presence of transplanted BMSCs in the liver tissue was analyzed by staining OV cells using a biotinylated anti-OV-6 antibodies followed by universal diaminobenzidine tetrahydrochloride (DAB) immunostaining detection kit. The standard avidin-biotin immunoperoxidase technique was used [25].
Liver function parametersSerum albumin concentration: Formation of albumin/bromcresol-green complex at pH 4.2 and photometric measurement of the absorbance were detected by the Biodiagnostic kits [26].
Aminotransferase enzymes (ALT, AST): The alanine aminotransferase (ALT) and aspartate aminotransferase (AST) activities were determined in serum using the Biodiagnostic kit [27].
Alkaline phosphatase (ALP) activity: ALP was determined in serum according to the method described by Belfield and Goldberg [28], using the Biodiagnostic test kit.
Statistical analysisThe statistical analysis was performed using the SAS, ver.9.2 software program. Data were summarized as mean±standard error (SE) for values and percentages. For comparison of more than 2 groups, the analysis of variance, ANOVA test, was used. Comparison between percentages was calculated by the chi-square test. Significant differences between means were determined by Duncan Post Hoc test [29]. P<0.05 implies a statistically significant difference.
RESULTSPCR detection of male-derived BMSCsThe sry gene that was used as the Y chromosome marker was detected in the liver tissue from the Schistosoma-BMSCs groups and Schistosoma-BMSCs-HGF groups, but not in the infected control or uninfected negative control groups (Fig. 1).
Liver function parametersThe performance of the liver was monitored by the serum level of liver proteins and enzymes as presented in Table 2 and Figs. 4, 5. At the 1st month PT, both groups treated with BMSCs only and BMSCs supplemented with HGF showed non-significant increases in serum albumin concentration as compared to the infected control group. At the 2nd and 3rd month PT, the albumin concentration in sera of mice treated with BMSCs and BMSCs supplemented with HGF increased significantly (P<0.05) compared to the infected control group.
At the 1st month PT with both BMSCs only and BMSCs supplemented with HGF, there were significant reductions (P<0.05) in both ALT and ALP activities, whereas, this reduction was non-significant in serum AST activity as compared to the infected control group. At the 2nd and 3rd month PT, the activities of ALT, ALP, and AST in sera of mice treated with BMSCs and BMSCs supplemented with HGF was reduced significantly (P<0.05) in comparison with that of the infected control group.
Detection of OV-6 in hepatic tissues using immunohistochemical techniqueThe presence of OV-6 in liver sections of normal, S. mansoni-infected mice, and infected mice treated with BMSCs and BMSCs supplemented with HGF was detected immunohistochemically using monoclonal anti-mouse OV-6 antibodies as a marker for newly formed hepatocytes differentiated from BMSCs. Normal uninfected negative control and S. mansoni-infected control mice showed negative expression of OV-6 in hepatocytes and granuloma cells.
At treatment with BMSCs only and BMSCs in combination with HGF, positively stained hepatocytes with brown colour appeared indicating the presence of newly formed hepatocytes. As the period after treatment with BMSCs increased, the expression of OV-6 in hepatocytes also increased. The greatest increase in the expression of OV-6 was recorded in hepatocytes of mice treated with BMSCS at the 3rd month PT. The staining of cells occurred intercalated between mouse hepatocytes and around granulomas present either singly or in clusters (Figs. 16,17,18,19,20,21,22,23,24,25).
DISCUSSIONSchistosomiasis is a wide-spread chronic helminthic infection which contributes to death of over half a million people yearly. The Schistosoma-induced liver disease associated with granulomatous inflammation constitutes the most prevalent disease among Egyptians. The disease is characterized by disorganized proliferation of hepatocytes, excessive scarring, and excessive collagen deposition which lead to chronic liver failure. Hence, chronic schistosomiasis was selected as an experimental model of a chronic liver disease which allows evaluation of stem cell migration to sites of damage and their subsequent contribution to repair and host survival [8].
This study was intended to demonstrate the fate of murine BMSCs after inoculation into murine diseased liver, in an attempt to set an experimental model of in vivo hepatocyte differentiation from BMSCs.
Previous studies have revealed that the intensity of schistosomal infection is related to the degree of liver fibrosis and granulomatous reaction [30]. The number of granulomas was correlated with the severity of the disease. As granulomas develop in response to egg deposition in the tissue, it can be possible to assess the amount of eggs retained in the liver and intestine [8]. This is in agreement with the present histopathological finding which was confirmed by the increased number and diameter of granuloma, number of liver and intestinal eggs, and extensive accumulation of fibrous tissues.
After treatment with BMSCs alone or in combination with HGF, there was an improvement in the histopathological picture of the liver which included diminution in the number and diameter of granulomas and reduction in the fibrotic content. Similar to the present findings, Abdel Aziz et al. [13] focused on the antifibrotic effect of mesenchymal stem cells (MSCs) on the liver of S. mansoni-infected mice. In their model, once granulomas were formed around the S. mansoni ova, the rate of spontaneous change of the collagen content of the granuloma was low, thereby providing a relatively stable in vivo model for analyzing collagen turnover. The histopathological examination of the liver of the S. mansoni-infected mice showed characteristic granulomas, which were cellular and contained thick collagen bands. After MSCs infusion, the granulomas decreased in size and number and became less cellular, although the concentric fibrous bands were still discernible.
In our study, the extent of fibrosis was estimated by the quantitative morphometric analysis of the collagen content in Sirius red stained liver sections. The results revealed significant decreases in the collagen content after treatment with BMSCs alone or in combination with HGF. In this regard, Ghanem et al. [8] demonstrated that fibrosis developed during the chronic phase of granulomatous inflammation in murine schistosomiasis and it represented a protective function during infection by neutralization and sequencing egg antigens that can potentially damage host tissues. The inhibitory effect of inoculated BMSCs on the collagen deposition may be related to an enhancement of fibrotic degradation rather than a decrease in fibrosis synthesis.
Pretreatment with MSCs [30] significantly reduced liver fibrosis compared to untreated cells. Antifibrotic effects of MSCs have been previously documented by many authors [31,32], and this might have a contributing factor for the observed decline in the liver fibrosis. A significant reduction of collagen content [13] estimated by Sirius red staining in MSCs infusion group was recorded as compared to the PI control values. They [13] also reported that resorption of fibrous tissues was observed from the first month post BMSCs administration. This was more rapid than fibrous tissue resorption observed with anti-Schistosoma drug treatment, where resorption started 3 months after the treatment.
Oval cells are hepatic precursors of hepatocytes and bile duct cells. The OV cells originated from BMSCs [33]. Chronic viral hepatitis was investigated [34], and it was noted that similar hepatic OV cells were allocated predominantly in the periportal region and fibrosis septa, characterized by an ovoid nucleus, small size, and scanty cytoplasm. In a study carried out to investigate the potential of BMSCs in regeneration of hepatic lesions induced by S. mansoni chronic infection [1], it was reported that transplanted cells migrated to granuloma areas and the cytokine level associated with fibrosis deposition in liver fragments of mice submitted to therapy was reduced. They also reported that infection with S. mansoni caused an increase in the number of OV cells which were mainly found in periportal areas of the hepatic lobe in saline-treated as well as BMSCs-treated mice.
The results of the current study showed that OV cells constituted the dominant forms of newly formed cells observed in the grids of the treated group. Stem cells in this study had plenty of time to develop and differentiate as the experiment last for 3 moths post transfection with BMSCs. On the contrary, another author reported that inoculated stem cells lasted for hours after the acute liver injury [35,36].
In our study, there was an increase in OV cell number in liver sections of different study groups. Using the anti-mouse OV-6 marker, the liver sections of treated groups either with BMSCs or with BMSCs supplemented with HGF showed positive staining results with increase in the number of cells. Negative reaction for OV-6 marker was noticed in the liver sections of either normal uninfected negative control group or infected untreated groups.
S. mansoni infection resulted in a hepatocellular injury, which in turn led to a release of enzymes from the injured hepatic cells into blood circulation [37]. In this regard, serum biochemical profiles in terms of ALT, AST, ALP, and albumin provided supportive evidence to the pathological alterations observed in response to schistosomal infection.
Aminotransferases are considered as marker enzymes for cell toxicity and their elevated level in serum give an additional support for S. mansoni cytotoxicity. Consistent with previous studies, the present study showed that the inflammatory reactions induced in the livers of S. mansoni-infected mice were ensured by liver dysfunctions reflected by elevated serum levels of ALT, AST, and ALP. These high serum concentrations of ALT and AST were attributed to the hepatocellular damage resulting from egg deposition where the transaminase levels showed an intimate relationship with cell necrosis and/or increased cell membrane permeability to discharge of the enzyme to the blood stream [38].
Many authors attributed the elevated level of ALP to irritation of liver cells by toxins or metabolites from growing schistosomules and eggs or due to a loss of intracellular enzymes by diffusion through the cell membrane which appeared to act as a stimulus to the synthesis of more enzymes, which would in turn increase the rate of diffusion and hence increase the serum enzyme activity [39,40].
In the present study, supplementation of BMSCs effectively ameliorated the above serum marker levels characteristic of schistosomal hepatopathy, and the best results were observed at the 3rd month PT. S. mansoni infection causes hypoalbuminemia in mice, and this phenomenon occurs simultaneously with an increase in collagen deposition and could be associated with a decrease in albumin mRNA [41]. In the present study, albumin was clearly recognized in serum at the 3rd month PT, but the rate of collagen deposition in the tissue was not changed considerably. Therefore, it is recommended to follow up the results for longer periods PT.
Also, the present results were in accordance with Abdel-Rahim et al. [42] who reported that the low serum albumin level reflected an impaired protein synthesis due to liver destruction of parenchymal liver cells. The same results were also reported by Mahmoud et al. [43] who found a significant reduction in the albumin level due to S. mansoni infection.
After treatment with BMSCs, or BMSCs-HGF, the present results revealed significant increases in the serum albumin level at the 2nd and 3rd month PT in both groups as compared to the infected control group reaching normalization at the 3rd month PT. The autologous transplanted BMSCs may differentiate into hepatocytes, restore serum albumin, and suppress transaminase activity and liver fibrosis in the present experimental model of liver injury. There were borderline significant improvements in the serum albumin level of the transplanted group compared to the control group at the end of the 6th month PT [12].
A significant reduction in the serum ALP level was observed [44] in experimental animals transplanted with pretreated MSCs compared to the controls. The level of serum ALP has been used previously as an indicator of improved liver functions.
The increase in albumin and decrease in ALT and AST levels in the serum are indicative of normalization of the liver function by MSCs treatment [45]. The reversal of the functional parameters of the fibrotic liver could be either due to prevention of apoptosis of parenchymal cells or inhibition of proliferation and infiltration of inflammatory cells.
In agreement with the present results, BM-MSCs infused intravenously were localized to the liver and resulted in improvement of liver functions [13]. The improvement of liver functions has been observed with or without prior expansion, fractionation, and cloning of the MSCs or their differentiation into hepatocyte-like cells in culture. On the other hand, 4 weeks after BMSCs transplantation to mice with liver fibrosis induced by CCl4 administration, the mice showed significant reduction in liver fibrosis as assessed by improvement of liver functions, such as albumin and bilirubin levels and prothrombin time [46].
In conclusion, generally BMSCs with or without HGF infusion significantly enhanced hepatic regeneration and alleviated hepatic fibrosis in a S. mansoni-induced fibrotic liver model and has therapeutic effects which appeared in reduction of immunopathology, granuloma formation, and hepatic fibrosis related to S. mansoni infection. Therefore, it is important to use different types of stem cell factors other than HGF to show if there is a considered difference in the liver regeneration intensity. This infusion could generate new hepatocytes to improve the function of residual hepatocytes. Therefore, autologous BMSCs transplantation may be considered as a curative or supportive therapy for liver disorders.
REFERENCES1. Oliveira SA, Souza BS, Guimarães-Ferreira CA, Barreto ES, Souza SC, Freitas LA, Ribeiro-Dos-Santos R, Soares MB. Therapy with bone marrow cells reduces liver alterations in mice chronically infected by Schistosoma mansoni. World J Gastroenterol 2008;14:5842-5850. PMID: 18855983.
2. Lorenzini S, Gitto S, Grandini E, Andreone P, Bernardi M. Stem cells for end stage liver disease: how far have we got? World J Gastroenterol 2008;14:4593-4599. PMID: 18698672.
3. Farci P, Roskams T, Chessa L, Peddis G, Mazzoleni AP, Scioscia R, Serra G, Lai ME, Loy M, Caruso L, Desmet V, Purcell RH, Balestrieri A. Long-term benefit of interferon α therapy of chronic hepatitis D: regression of advanced hepatic fibrosis. Gastroenterology 2004;126:1740-1749. PMID: 15188169.
4. Satapathy SK, Sakhuja P, Malhotra V, Sharma BC, Sarin SK. Beneficial effects of pentoxifylline on hepatic steatosis, fibrosis and necroinflammation in patients with non-alcoholic steatohepatitis. J Gastroenterol Hepatol 2007;22:634-638. PMID: 17444848.
5. Mathew RC, Boros DL. Regulation of granulomatous inflammation in murine schistosomiasis. III. Recruitment of antigen-specific I-J+ T suppressor cell of the granulomatous response by I-J+ soluble suppressor factor. J Immunol 1986;136:1093-1097. PMID: 2416827.
6. Baddamwar A. Report no. 46. ISSN. Hepatic fibrosis in experimental Schistosoma japonicum infection in pigs: a histopathological and immunohistochemical study. Uppsala, Sweden. Swedish University of Agricultural Sciences. 2004, pp 1403-2201.
7. Phillips SM, Colley DG. Immunologic aspects of host response to schistosomiasis: resistance, immunopathology, and eosinophil involvement. Prog Allergy 1978;24:49-82. PMID: 78498.
8. Ghanem LY, Dahmen U, Dirsch O, Nosseir MM, Mahmoud SS. Does granulocyte-colony stimulating factor administration induce damage or repair response in schistosomiasis? World J Hepatol 2010;2:434-441. PMID: 21191519.
9. Dinarello CA, Cannon JG, Wolff SM, Bernheim HA, Beutler BA, Cerami A, Figari I, Palladino MA Jr, O'Connor JV. Tumor necrosis factor (cachectin) is an endogenous pyrogen and induces production of interleukin 1. J Exp Med 1986;163:1433-1450. PMID: 3486936.
10. Pan Y, Dong S, Hao Y, Zhou Y, Ren X, Wang J, Wang Y, Chu T. Ultrasonic-assisted extraction process of crude polysaccharides from Yunzhi mushroom and its effect on hydroxyproline and glycosaminoglycan levels. Carbohydr Polym 2010;81:93-96.
11. Reddy GK, Enwemeka CS. A simplified method for the analysis of hydroxyproline in biological tissues. Clin Biochem 1996;29:225-229. PMID: 8740508.
12. Salama H, Zekri AR, Bahnassy AA, Medhat E, Halim HA, Ahmed OS, Mohamed G, Al Alim SA, Sherif GM. Autologous CD34+ and Cd133+ stem cells transplantation in patients with end stage liver disease. World J Gastroenterol 2010;16:5297-5305. PMID: 21072892.
13. Mt AA, Atta HM, Roshdy NK, Rashed LA, Sabry D, Hassouna AA, Aboul Fotouh GI, Hasan NM, Younis RH, Chowdhury JR. Amelioration of murine Schistosoma mansoni induced liver fibrosis by mesenchymal stem cells. J Stem Cells Regen Med 2012;8:28-34. PMID: 24693190.
14. Pai M, Zacharoulis D, Milicevic MN, Helmy S, Jiao LR, Levicar N, Tait P, Scott M, Marley SB, Jestice K, Glibetic M, Bansi D, Khan SA, Kyriakou D, Rountas C, Thillainayagam A, Nicholls JP, Jensen S, Apperley JF, Gordon MY, Habib NA. Autologous infusion of expanded mobilized adult bone marrow-derived CD34+ cells into patients with alcoholic liver cirrhosis. Am J Gastroenterol 2008;103:1952-1958. PMID: 18637092.
15. Alison MR, Poulsom R, Jeffery R, Dhillon AP, Quaglia A, Jacob J, Novelli M, Prentice G, Williamson J, Wright NA. Hepatocytes from non-hepatic adult stem cells. Nature 2000;406:257. PMID: 10917519.
16. Braun KM, Sandgren EP. Cellular origin of regenerating parenchyma in a mouse model of severe hepatic injury. Am J Pathol 2000;157:561-569. PMID: 10934158.
17. Lagasse E, Connors H, Al-Dhalimy M, Reitsma M, Dohse M, Osborne L, Wang X, Finegold M, Weissman IL, Grompe M. Purified hematopoietic stem cells can differentiate into hepatocytes in vivo. Nat Med 2000;6:1229-1234. PMID: 11062533.
18. Bartlett JM, Stirling D. A short history of the polymerase chain reaction. Methods Mol Biol 2003;226:3-6. PMID: 12958470.
19. Elkhafif N, Yehia H, Voss B, Hammam OA, Akl M, Mansy S, Mahmoud S, El Bendary O, El Fandy G. Differentiation and homing of transplanted bone marrow cells in livers of murine schistosomiasis: Pilot study. Aust J Basic Appl Sci 2008;2:1362-1372.
20. Elkhafif N, Voss B, Hammam O, Yehia H, Mansy S, Akl M, Boehm S, Mahmoud S, El Bendary O, El Fandy G. Homing of transplanted bone marrow cells in livers of Schistosoma mansoni-infected mice. APMIS 2010;118:277-287. PMID: 20402673.
21. Mahmoud AAF, Warren KS. Anti-inflammatory effects of tartar emetic and niridazole: suppression of Schistosoma egg granuloma. J Immunol 1974;112:222-228. PMID: 4855830.
22. Boros DL, Warren KS. Delayed hypersensitivity-type granuloma formation and dermal reaction induced and elicited by a soluble factor isolated from schistosomiasis mansoni eggs. J Exp Med 1970;132:488-507. PMID: 5535626.
23. Mohamed AM, Mahmoud SS, Farrag AA. Influence of sative seeds against liver fibrosis and consequence complications in murine schistosomiasis. Int J Biotech Bioche 2008;4:325-346.
24. Junqueira LC, Bignolas G, Brentani RR. Picrosirius staining plus polarization microscopy, a specific method for collagen detection in tissue sections. Histochem J 1979;11:447-455. PMID: 91593.
25. Hsu SM, Raine L. Protein A, avidin, and biotin in immunohistochemistry. J Histochem Cytochem 1981;29:1349-1353. PMID: 6172466.
26. Dumas BT, Watson WR. Albumin standard and the measurement of serum albumin with bromcresol green. Clin Chim Acta 1997;258:21-30. PMID: 9049440.
27. Reitman S. A colorimertic method for the determniation of serum glutamic oxalacetic and glutamic pyruvic transaminases. Am J Clin Pathol 1957;28:56-63. PMID: 13458125.
28. Belfield A, Goldberg DM. Hydrolysis of adenosine-monophosphate by acid phosphatase as measured by a continuous spectrophotometric assay. Enzyme 1971;12:561-566. PMID: 5169852.
30. Mohsin S, Shams S, Ali Nasir G, Khan M, Javaid Awan S, Khan SN, Riazuddin S. Enhanced hepatic differentiation of mesenchymal stem cells after pretreatment with injured liver tissue. Differentiation 2011;81:42-48. PMID: 20943307.
31. Zhao DC, Lei JX, Chen R, Yu WH, Zhang XM, Li SN, Xiang P. Bone marrow-derived mesenchymal stem cells protect against experimental liver fibrosis in rats. World J Gastroenterol 2005;11:3431-3440. PMID: 15948250.
32. Abdel Aziz MT, Atta HM, Mahfouz S, Fouad HH, Roshdy NK, Ahmed HH, Rashed LA, Sabry D, Hassouna AA, Hasan NM. Therapeutic potential of bone marrow-derived mesenchymal stem cells on experimental liver fibrosis. Clin Biochem 2007;40:893-899. PMID: 17543295.
33. Petersen BE, Bowen WC, Patrene KD, Mars WM, Sullivan AK, Murase N, Boggs SS, Greenberger JS, Goff JP. Bone marrow as a potential source of hepatic oval cells. Science 1999;284:1168-1170. PMID: 10325227.
34. Ma X, Qiu DK, Peng YS. Immunohistochemical study of hepatic oval cells in human chronic viral hepatitis. World J Gastroenterol 2001;7:238-242. PMID: 11819767.
35. Sell S. Electron microscopic identification of putative liver stem cells and intermediate hepatocytes following periportal necrosis induced in rats by allyl alcohol. Stem Cells 1997;15:378-385. PMID: 9323801.
36. Sell S. Heterogeneity and plasticity of hepatocyte lineage cells. Hepatology 2001;33:738-750. PMID: 11230756.
37. Hanna LS, Medhat AM, Abdel-Menem HA. Biochemical changes after subchronic and chronic interaction of Schistosoma mansoni infection in Swiss albino mice with two specific compounds. J Egypt Soc Parasitol 2003;33:245-260. PMID: 12739815.
38. El-Rigal NS, Hetta MH. Effect of Citrus reticulata on serum protein fractions of mice after Schistosoma mansoni infection. J Appl Sci 2006;6:1447-1455.
39. El-Aasar AA, El-Merzabani MM, Zakhary NI, Farag HI, Abdeen AM, Abd El-Salam I, Mokhtar NM. Biochemical and biophysical studies on schistosomal liver of mice. Egypt J Bilharz 1989;11:19-33.
40. Abdel-Rahman HM, El-Shanawani FM, Hassan MM, Salem M, El-Sahly AM. Alkaline phosphatase isoenzymes abnormalities in hepatic schistosomiasis. Egypt J Bilharz 1993;15:41-48.
41. Saber MA, Shafritz DA, Zern MA. Changes in collagen and albumin mRNA in liver tissue of mice infected with Schistosoma mansoni as determined by in situ hybridization. J Cell Biol 1983;97:986-992. PMID: 6619195.
42. Abdel-Rahim IM, Kaiser C, Homeida MA, Elsheikh M, Schmidt E, Ehrich JH, Doehring-Schwerdfeger E. Enzyme activities and protein concentrations in serum of patients with hepatosplenic schistosomiasis. Trop Med Parasitol 1990;41:262-264. PMID: 1701559.
43. Mahmoud MR, El-Abhar HS, Saleh S. The effect of Nigella sativa oil against the liver damage induced by Schistosoma mansoni infection in mice. J Ethnopharmacol 2002;79:1-11. PMID: 11744288.
44. El-Lakkany NM, Seif-El-Din SH, Badawy AA, Ebeid FA. Effect of artemether alone and in combination with grapefruit juice on hepatic drug-metabolizing enzymes and biochemical aspects in experimental Schistosoma mansoni. Int J Parasitol 2004;34:1405-1412. PMID: 15542101.
45. Pulavendran S, Vignesh J, Rose C. Differential anti-inflammatory and anti-fibrotic activity of transplanted mesenchymal vs. hematopoietic stem cells in carbon tetrachloride-induced liver injury in mice. Int Immunopharmacol 2010;10:513-519. PMID: 20144743.
46. Sakaida I, Terai S, Yamamoto N, Aoyama K, Ishikawa T, Nishina H, Okita K. Transplantation of bone marrow cells reduced CCl4-induced liver fibrosis in mice. Hepatology 2004;40:1304-1311. PMID: 15565662.
Fig. 1UV transilluminated agarose gel of PCR products of sry gene. Lane 1, PCR marker; lane 2, normal group; lane 3, infected group; lane 4, BMSCs treated group; lane 5, BMSCs-HGF treated group. 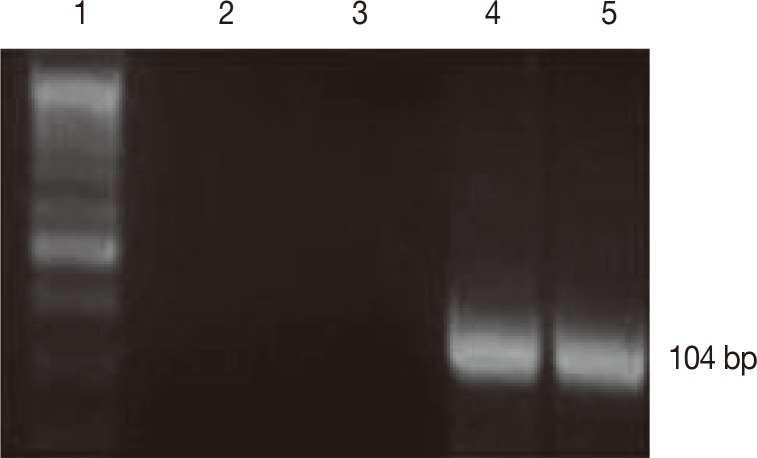
Fig. 2Effect of BMSCs and BMSCs-HGF treatments on mean hepatic granuloma diameter in infected and treated groups. MGD, mean granuloma diameter. 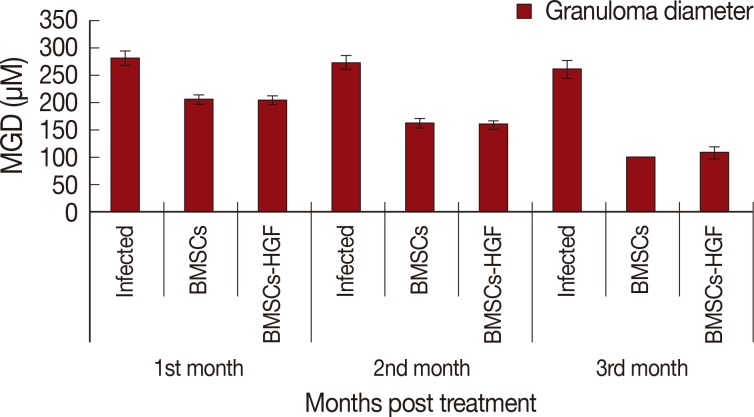
Fig. 3Effect of BMSCs and BMSCs-HGF treatment on mean hepatic granuloma count in infected and treated groups. 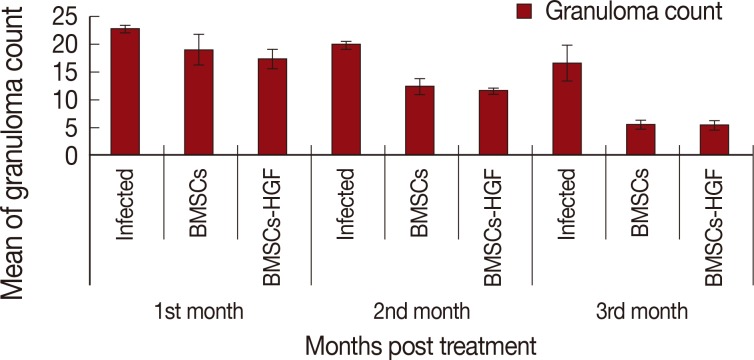
Fig. 4Effect of BMSCs and BMSCs-HGF on serum albumin level of Schistosoma mansoni-infected mice in different studied groups. 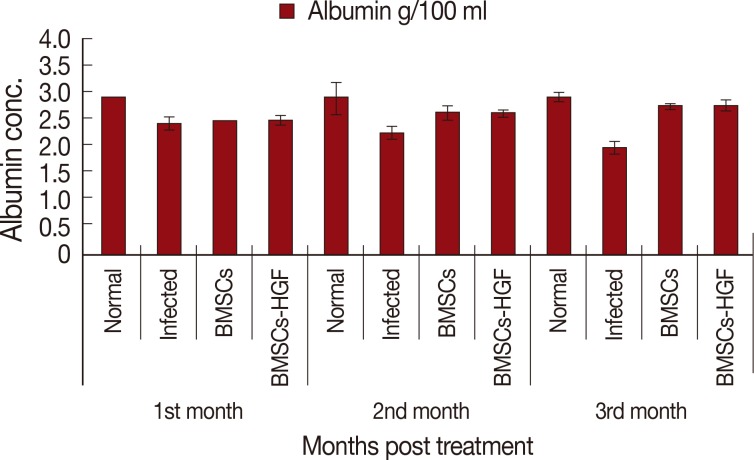
Fig. 5Effect of BMSCs and BMSCs-HGF on serum ALT, AST, and ALP levels of Schistosoma mansoni-infected mice in different studied groups. 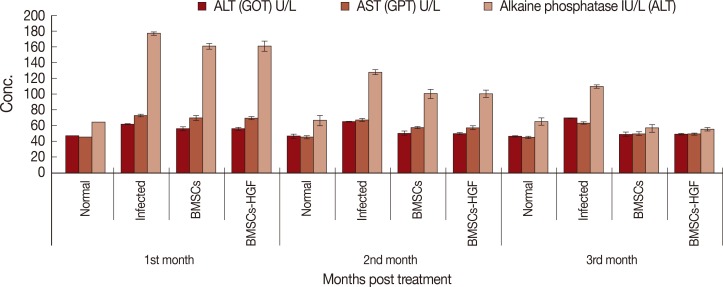
Fig. 7Liver tissue section of infected control mice at week 12 PI showing a large fibrocellular granuloma surrounded by pink-red dense collagen bundles (Sirius Red, ×200). 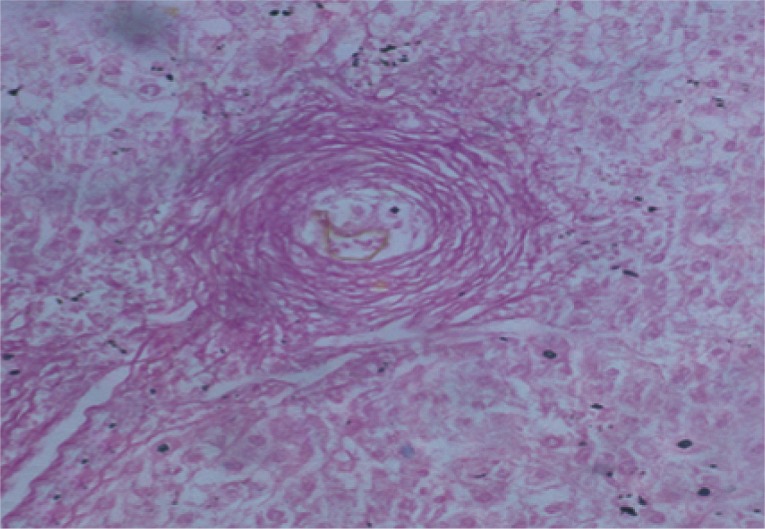
Fig. 8, 9Liver tissue sections of BMSCs and BMSCs-HGF recipient female mice at the 1st month post treatment showing a medium fibrocellular granuloma with red-stained concentric collagen bundles (Sirius Red, ×200). 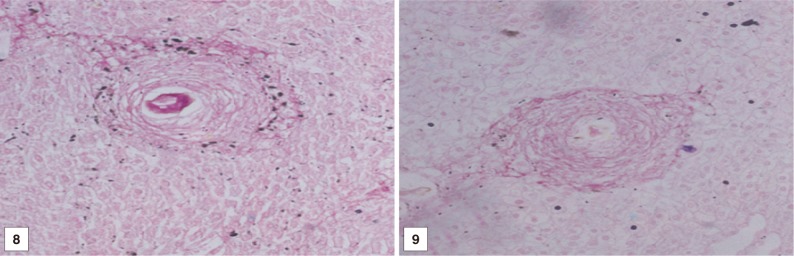
Fig. 10Liver tissue section of infected control mice at week 16 PI showing a medium fibrocellular granuloma surrounded by red-stained concentric collagen bundles (Sirius Red, ×200). 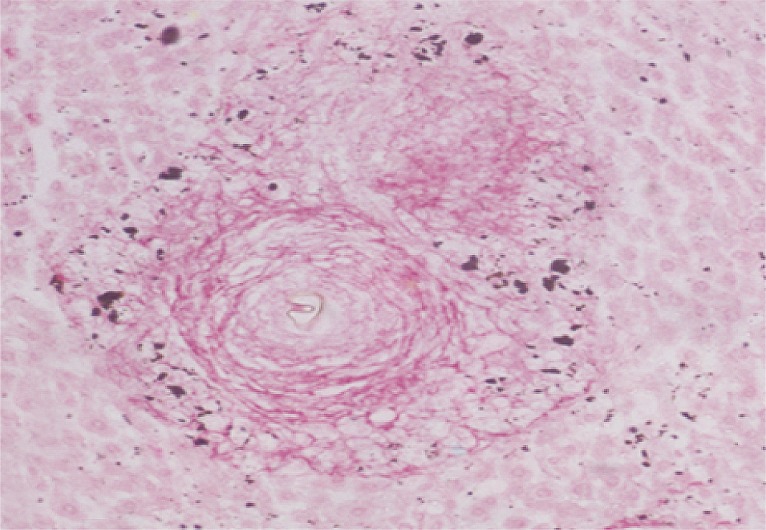
Fig. 11, 12Liver tissue sections of BMSCs and BMSCs-HGF recipient female mice at the 2nd month post treatment showing a small fibrocellular granuloma surrounded the parasite's ovum with scattered concentric red-stained collagen bundles (Sirius Red, ×200). 
Fig. 13Liver tissue section of infected control mice at week 20 PI showing a characteristic large fibrocellular granuloma surrounded the parasite's ovum with dense red-stained collagen bundles (Sirius Red, ×200). 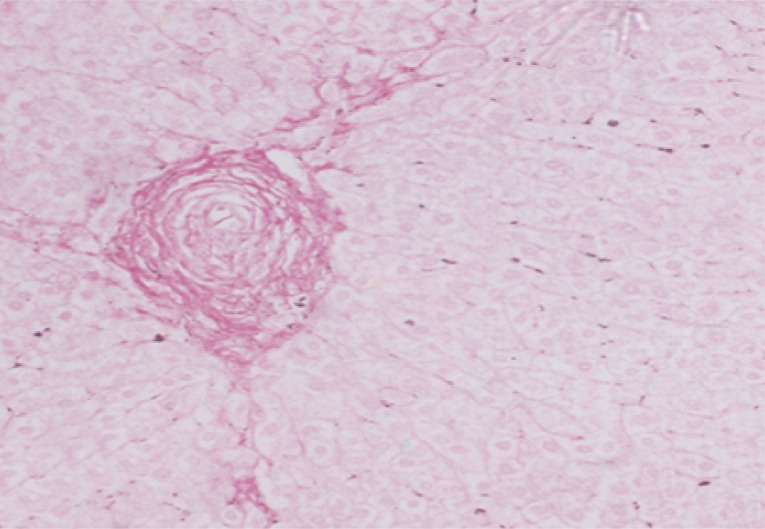
Fig. 14, 15Liver tissue sections of BMSCs and BMSCs-HGF recipient female mice at the 3rd month post treatment showing a diminished fibrocellular granuloma surrounded the parasit's ovum with scattered concentric red-stained collagen bundles (Sirius Red, ×200). 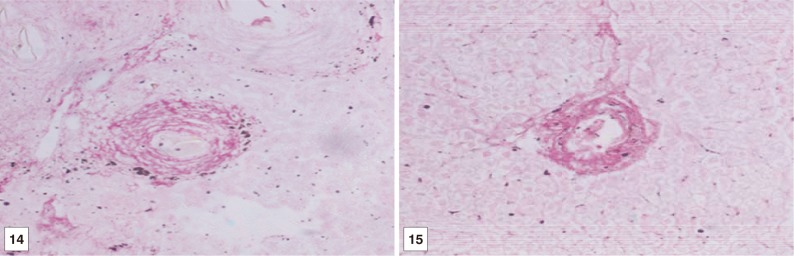
Fig. 16Immunostain for OV-6 antibody (DAB, ×200) in a liver section of normal uninfected negative control mice showing negative expression for OV-6 monoclonal antibody. 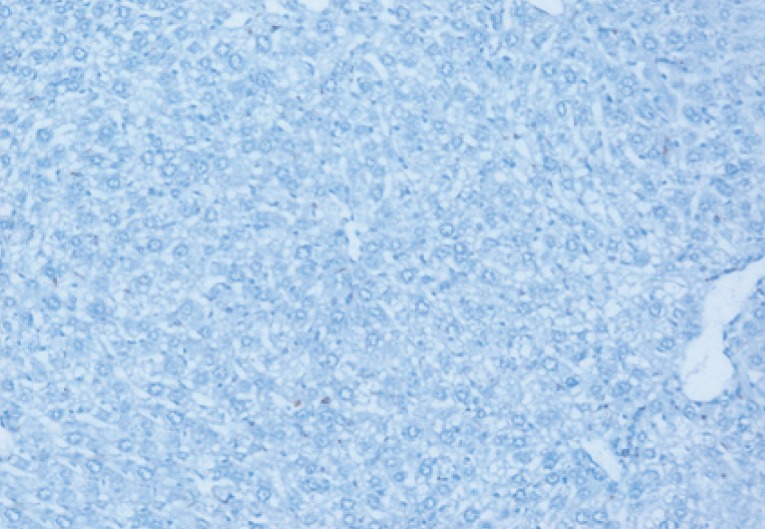
Fig. 17Immunostain for OV-6 antibody (DAB, ×200) in a liver section of infected control mice at week 12 PI showing negative expression of OV-6 monoclonal antibody in hepatocytes and granuloma cells. 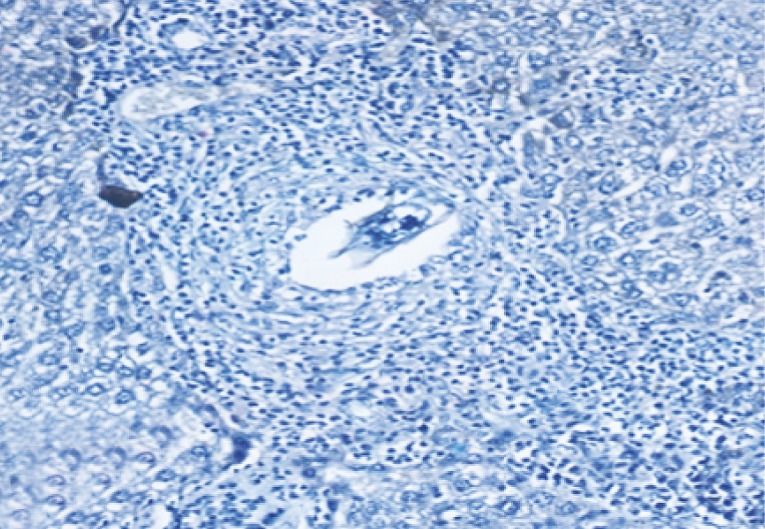
Fig. 18, 19Immunostain for OV-6 antibody (DAB, ×200) in liver sections of BMSCs and BMSCs-HGF recipient female mice at the 1st month post treatment showing markedly mild expression of OV-6 monoclonal antibody (as cytoplasmic brown colour) in hepatocytes like cells and granuloma cells. 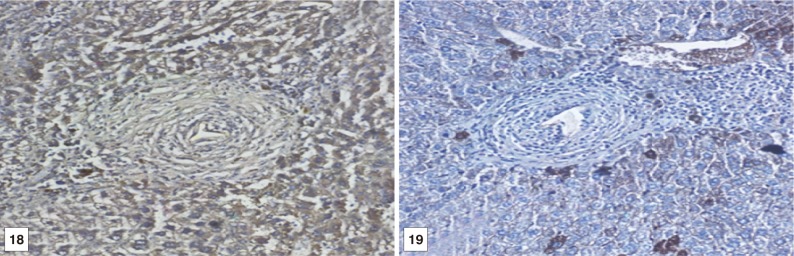
Fig. 20Immunostain for OV-6 antibody (DAB, ×200) in a liver section of infected control mice at week 16 PI showing negative expression of OV-6 monoclonal antibody in hepatocytes and granuloma cells. 
Fig. 21, 22Immunostain for OV-6 antibody (DAB, ×200) in liver sections of BMSCs and BMSCs-HGF recipient female mice at the 2nd month post treatment showing marked and mild expression of OV-6 monoclonal antibody (as cytoplasmic brown colour) in hepatocytes like cells and granuloma cells. 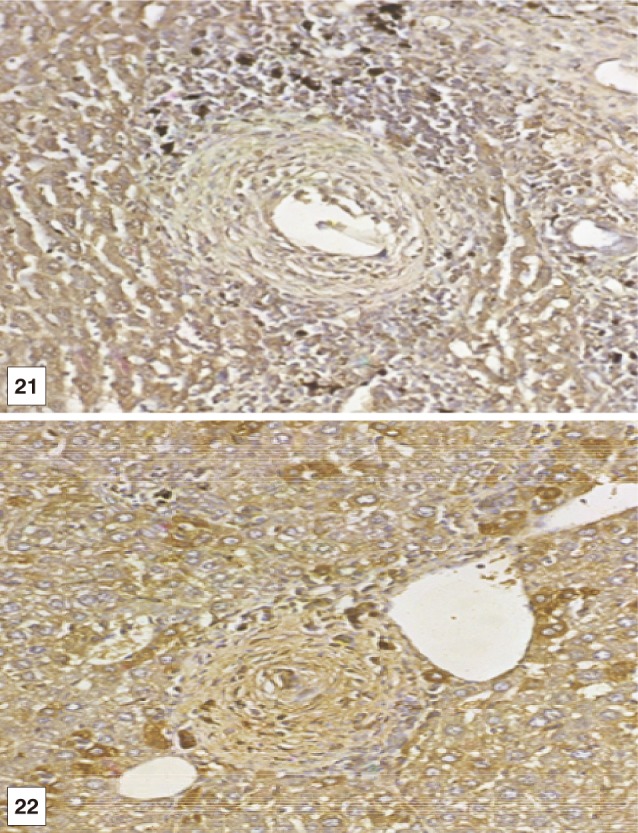
Fig. 23Immunostain for OV-6 antibody (DAB, ×200) in a liver section of infected control mice at week 20 PI showing negative expression of OV-6 in hepatocytes and granuloma cells. 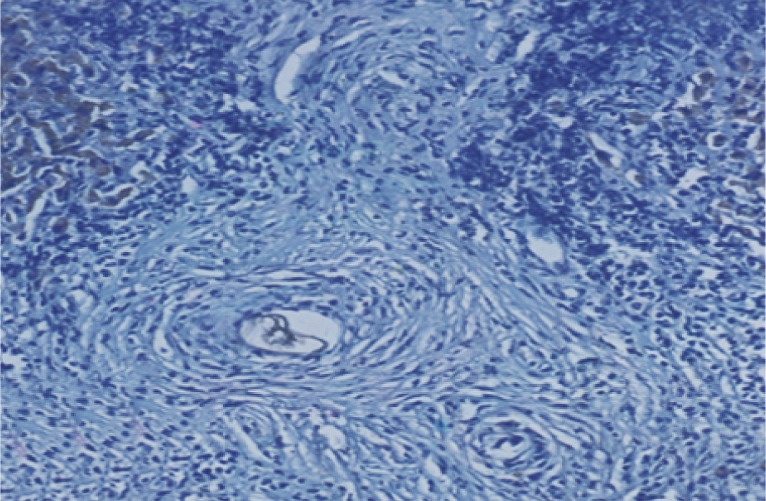
Fig. 24, 25Immunostain for OV-6 antibody (DAB, ×200) in liver sections of BMSCs and BMSCs-HGF recipient female mice at the 3rd month post treatment showing marked and mild expression of OV-6 monoclonal antibody (as cytoplasmic brown colour) in hepatocytes like cells and granuloma cells. 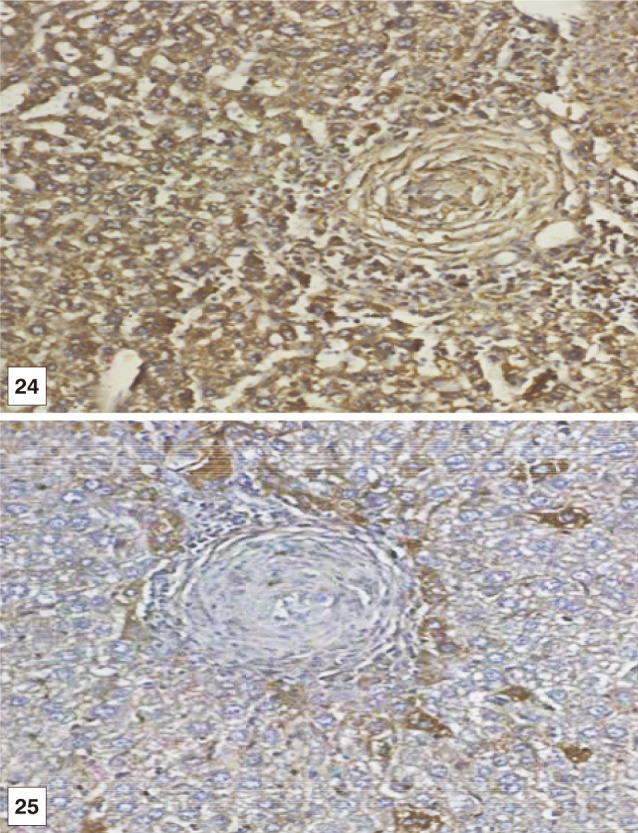
Table 1.Effect of treatment with BMSCs and BMSCs-HGF on mean hepatic granuloma diameter and number of mice Table 2.Effect of treatment with BMSCs and BMSCs-HGF on the serum concentration of liver albumin and activities of ALT, AST, and ALP of mice |
|
|||||||||||||||||||||||||||||||||||||||||